Psychological Crash After Cocaine Use

posted 28th January 2026
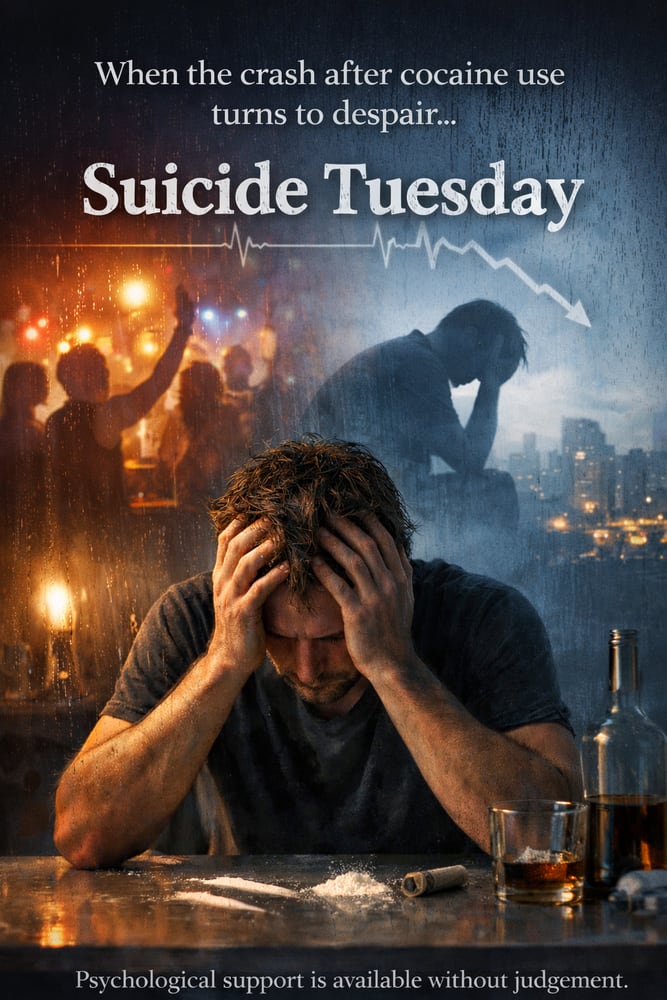
“Suicide Tuesday”: Understanding the Psychological Crash After Cocaine Use
In clinical practice, some patterns emerge quietly but consistently. One such pattern is the emotional collapse that can follow a weekend of cocaine use, often peaking not immediately, but days later. Clients describe a familiar sequence: heightened confidence and energy during the weekend, followed by exhaustion on Monday, and then, by Tuesday, a profound emotional low. For some, this includes intrusive thoughts, overwhelming shame, hopelessness, and in more severe cases, thoughts of suicide. Informally, this experience has become known as “Suicide Tuesday.” While not a diagnostic term, it reflects a real and clinically recognised phenomenon that warrants serious attention.
Cocaine’s psychological effects are driven largely by its impact on the brain’s dopamine system. Dopamine plays a central role in motivation, anticipation, confidence, and the sense that life feels rewarding and meaningful. During cocaine use, dopamine levels rise sharply, often producing feelings of clarity, connection, emotional relief, and heightened self-belief. For individuals who are stressed, self-critical, or emotionally constrained, this state can feel like a temporary return to themselves.
What is less visible is the cost that follows. The brain responds to artificially elevated dopamine by reducing receptor sensitivity, a process known as downregulation. Once the drug wears off, dopamine activity does not simply return to baseline; it often drops below it. This creates a state of dopaminergic depletion, where motivation collapses and the emotional tone of life shifts abruptly. The result is not just a comedown, but a temporary loss of meaning, pleasure, and psychological resilience.
For some individuals, this post-cocaine state is intensely destabilising. People often report intrusive negative thoughts, emotional emptiness, heightened anxiety, and a harsh internal narrative characterised by shame and self-condemnation. Thoughts such as “I’ve ruined everything,” “This proves I’m broken,” or “I can’t face my life” become louder during this period. From a clinical perspective, these thoughts emerge at a time when emotional regulation is compromised and reward systems are offline, making distress feel both urgent and inescapable.
Within diagnostic frameworks such as the DSM-5-TR, this presentation may fall under Substance-Induced Depressive Disorder. The depressive symptoms are directly linked to substance use, but that does not make them mild, imagined, or insignificant. For individuals with pre-existing vulnerabilities, including depression, trauma histories, or impulsivity, this neurochemical crash can significantly increase suicide risk.
The timing of this emotional low is not accidental. Cocaine’s immediate effects are short-lived, but the neurochemical and psychological consequences unfold over several days. By Tuesday, sleep deprivation has accumulated, serotonin and dopamine levels are at their lowest, and the protective buffer of weekend distraction has disappeared. Practical realities return — work, responsibilities, relationships — often accompanied by regret or consequences linked to substance use. The collision of biological depletion and psychological reckoning can be overwhelming.
Shame plays a particularly dangerous role in this process. Many individuals judge themselves harshly for using drugs, for losing control, or for feeling emotionally fragile afterward. This self-judgement often prevents people from reaching out for support at precisely the moment they are most vulnerable. Clinically, it is important to recognise that this state is not a moral failure or a lack of character. It is a predictable response of a nervous system under strain, compounded by self-criticism.
Importantly, this phenomenon is not limited to people with chaotic or long-term substance misuse. Many individuals experiencing “Suicide Tuesday” are outwardly high-functioning, successful, and socially integrated. Cocaine use may be intermittent, framed as recreational, or tied to social or professional environments. Because their lives appear stable, the intensity of the emotional crash can feel especially confusing and frightening. The contrast between external success and internal collapse often deepens distress and self-doubt.
Understanding this pattern is essential for prevention. Awareness of the neuropsychological effects of stimulant use can reduce fear and stigma, and help individuals recognise that the emotional crash is not permanent. Clinically, risk can be reduced by limiting or eliminating cocaine use, avoiding alcohol during recovery periods, prioritising sleep, and seeking support rather than withdrawing into isolation. When this pattern repeats, it should be taken seriously as a signal that the nervous system is being overwhelmed.
Professional support is strongly advised when substance use is followed by persistent low mood, intrusive or frightening thoughts, or a sense of emotional instability that feels out of control. Therapy can help individuals understand why cocaine has become appealing, how the reward system has adapted, and how to reduce risk while rebuilding psychological stability. When suicidal thoughts are present, immediate help is essential. In the UK, support is available through NHS crisis services, Samaritans (116 123), or emergency services if there is imminent risk.
“Suicide Tuesday” is not about a particular day of the week. It is about what happens when neurobiology, emotion, and self-judgement collide in the absence of support. With education, compassion, and timely intervention, this risk is understandable — and preventable.